The Biopsychosocial Model: A Framework for Patient-Centric Healthcare Marketing
It’s widely taught by healthcare market research companies that there are two reasons to conduct market research: problem-seeking and problem-solving. As true as this may be, there’s a third reason that often remains unspoken—understanding.
Understanding is arguably the most important component of any successful healthcare marketing transaction, but unfortunately, it is often glossed over or misunderstood entirely.
Market research without understanding and context is like an empty coffee mug. It’s still a driving force behind your healthcare marketing strategy, but without understanding the patient experience, you lack the fuel needed for real movement. Understanding fuels thinking and aids you with the perspective of your stakeholders when designing marketing and patient support solutions.
Market research that is light on (or even void of) understanding and context risks being incomplete, leaving you, as the marketer, to fill in a large, under-the-surface gap. Before we ever start to discuss solutions or strategic design, it’s imperative that marketers strive to see the problem or area of focus through the eyes of the stakeholder.
Human Understanding or Bust
Using healthcare market research to illuminate a problem is one thing. Using healthcare research to understand that problem is altogether something else—and should be the only reason we conduct research. In today’s value-driven and patient-centric healthcare landscape, understanding the drivers behind problems—the socio-economic realities, ground-level stakeholder truths, and systematic shortcomings that create that problem in the first place—is critical to problem-solving.
There’s a reason patients do the things they do, and understanding those reasons through patient-centric healthcare marketing research is the quickest way to fostering relevant messaging that leads to better care and better outcomes. It’s sometimes not easy, but it’s worth the investment.
Understanding is difficult. It takes listening to and observing a range of stakeholders, such as family, caregivers, clinical staff, and other related stakeholders at ground level to identify and understand their lived experiences and the burdens of disease or treatment. This is where qualitative methods shine—helping illuminate patient needs, motivations, and realities, thereby adding value to the often abundant, yet insufficient quantitative data that so many hospital marketers depend on.
A balance of qualitative and quantitative data is your best bet if you want to cultivate deep understanding that will stand up to the demands of leadership while serving the strategy of your health system. By taking a mixed-methods approach to market research you will pave the way to understanding.
The Agency for Healthcare Research and Quality defines mixed methods as “… an emergent methodology of research that advances the systematic integration, or ‘mixing,’ of quantitative and qualitative data within a single investigation or sustained program of inquiry. The basic premise of this methodology is that such integration permits a more complete and synergistic utilization of data than do separate quantitative and qualitative data collection and analysis.”
Quantitative insights will provide cold hard data that is void of human context—the why behind the what. Understanding emerges when you take the time to listen and observe your patient at ground level. You must understand the situation in the market, understand the people behind the problems, understand the community’s opinion of those problems, and understand the hospital’s capabilities in addressing those problems. Then you have the type of understanding needed to effectively problem-solve.
Building a Better, More Empathic, and More Patient-Centric Healthcare Market Research Mousetrap
Virtually all hospitals have access to quantitative data (discharge, EHR data, reimbursement, market statistics, market surveys, and so on), but that type of data alone is not enough—integrating qualitative understanding with statistical data is the only logical way to illuminate a well-rounded picture. A mixed-methods approach provides balance and understanding that will fuel better strategies for connecting with, educating, and empowering patients and consumers to play a more active role in their health and well-being while also advancing the business strategy of the hospital and health system.
Healthcare marketers are being increasingly compelled to stop depending on, and acting on, purely statistics and numbers—healthcare marketers need to seek out and act on the deep stakeholder understanding that emerges when melding quantitative and qualitative insights. Marketers who rely solely on numbers will lose their strategic edge and ultimately market position in the face of healthcare marketing professionals who champion the human voice as a critical component of strategy.
In using a mixed-methods approach and employing empathic qualitative methods to dig deeper, you not only uncover problems in your hospital and community but understand why the problems exist at ground level through the patient experience.
The Innovation Adoption Curve Explains Our Slow Uptake of a Patient-Centric Approach
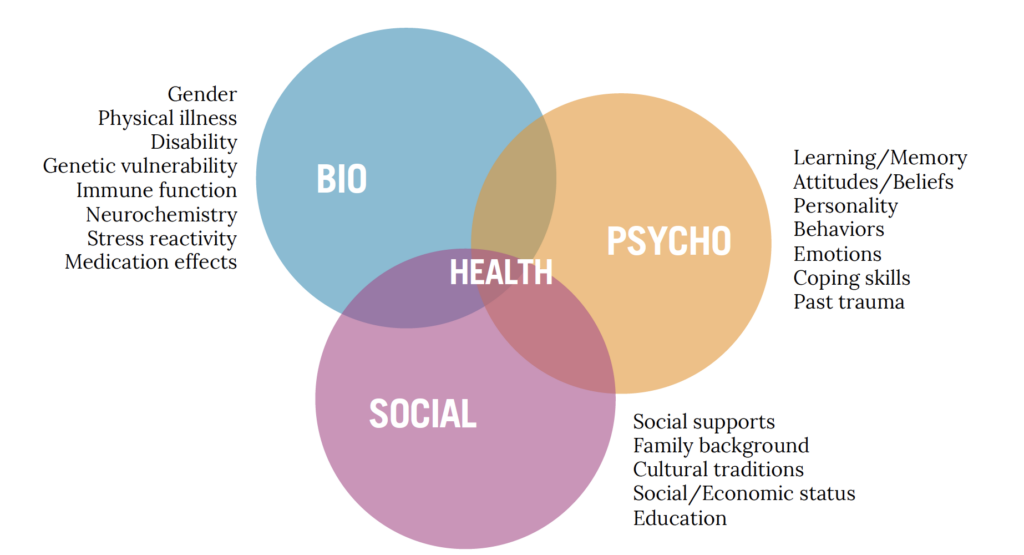
The next logical question is, if Engel developed his Biopsychosocial Model all the way back in the 1970s, why is the healthcare industry just now catching on to patient-centricity and holistic care? Great question.
Everett Rogers’ theory of innovation adoption partially accounts for the delay. for those unfamiliar, the theory purports that the process of adopting or accepting a new product or idea is lengthy. It takes the shape of a classic bell curve, and there are five groups along this curve:
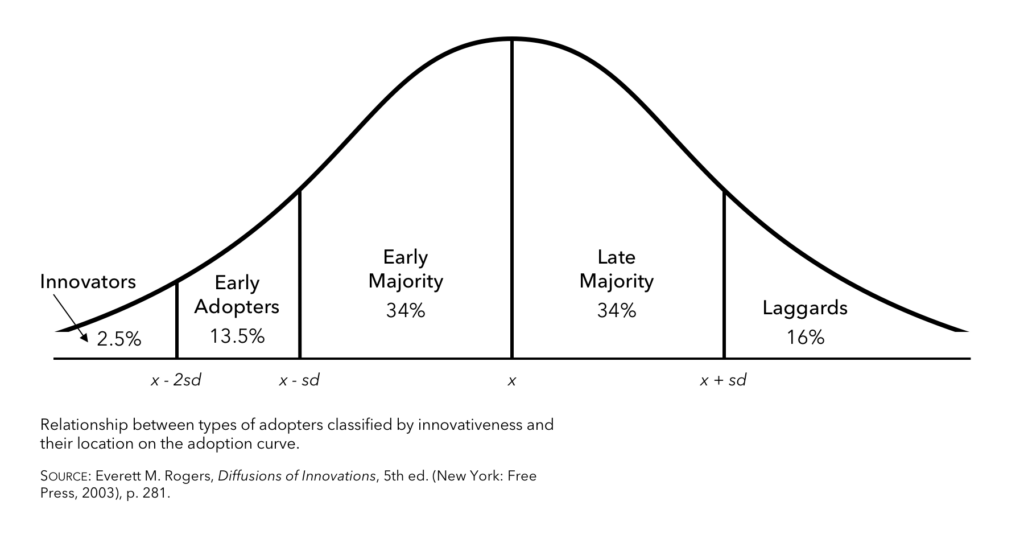
We don’t need to get into the weeds of this theory here. Just know that Engel is the innovator; he invented the Biopsychosocial Model. And because innovations are seen as risky by nature of their newness, society waits for other adopters to support innovations — new products, ideas, and technologies — before there’s widespread acceptance. It follows that, even though it’s been nearly 50 years, healthcare marketers and patient advocates are just now crossing that chasm between early adopters and the early majority.
The good news? As more and more healthcare industry players strive to understand the whole patient, we’re armed with more and more evidence of the efficacy of Engel’s innovation. The idea of patient-focused care becomes less intimidating, and, as we’re witnessing, adoption rate increases.
3 Recent Pieces of Healthcare Legislation That Have Ignited a Renewed Interest in Patient Understanding and Patient Centeredness
The Prescription Drug User Fee Act (PDUFA V)
The PDUFA was enacted in 1992 and reauthorized in 2012 as PDUFA V. Both the original law and the 2012 reauthorization sped up the delivery of life-saving medicines to patients. More specifically, the most recent reauthorization upgraded the benefit/risk assessments of new medicines and demanded inclusion of the patient voice in these drug review processes.
The 21st Century Cures Act
Passed in 2016, The 21st Century Cures Act emphasizes the need for patient engagement and offers a compelling case for the value of patient insights in the drug development and review process. Add this to PDUFA V and you’ve set the stage for patients to have a greater say in how pharmaceuticals are developed and marketed to them.
The Affordable Care Act
This discussion wouldn’t be complete without mention of the ACA, passed in 2010. The ACA certainly fell short in affecting wide-sweeping innovation or change, but it did facilitate two important steps toward a system that champions more than complexity:
- Compelling transparency. The ACA has moved the entire healthcare industry to be more transparent. Consumers can now see deeper into the system, glimpsing procedure costs, insurance coverages, and direct costs for the first time.
- Monitoring patient quality. Under the ACA, healthcare providers are penalized if they don’t meet certain preset quality of care metrics. What’s more, these metrics are rooted in patient satisfaction scores.
Let’s be clear: The ACA is far from perfect. That said, these two steps hold healthcare companies more accountable than before. Now, healthcare companies must maintain some level of quality when it comes to patient care for fear of government retribution.
Tying it All Together: The Overarching Implications for the Future of Patient-Centric Healthcare Marketing
Between the innovation adoption curve theory and recent legislation, it almost makes sense that Engel’s groundbreaking ideas weren’t truly at the forefront until recently. Even now, his Biopsychosocial Model and its patient-first approach are only just beginning their ascent. After all, we’re transitioning on Rogers’ bell curve from early adopters to early majority, when a larger percentage of the healthcare industry will accept patient-first care as their norm.
To avoid being a laggard on the other side of that curve, you need to act now. It’s the perfect time for you to increase focus on the patient and consumers. As a first step toward a more patient-focused healthcare company, the next time you’re planning clinical trials or developing a healthcare marketing strategy, get in front of your patients. Begin to understand, from a qualitative perspective, their lived reality by asking them about their illness journeys. Let that reality authentically inform decision-making for your company and you will see amazing results.
In Closing: A Final Tribute to George Engel
Even though patient-centric approaches are on the rise, Engel himself remains underappreciated for his role in its beginnings. But without his Biopsychosocial Model, we likely still wouldn’t take the patient’s “whole person” into consideration. The entire healthcare industry can benefit from Engel’s knowledge, and it’s time we recognize his contribution toward meeting our newfound patient-centric healthcare marketing goals.