Why Net Promoter Score Matters for Hospital Growth
Is NPS the Only Number You Need? Maybe.
Since Fred Reichheld introduced it in his 2003 Harvard Business Review article, “The One Number You Need to Grow,” the Net Promoter Score (NPS) has become a dominant measure of consumer loyalty and future growth potential. It’s simple, predictive, and powerful—which is why banks, airlines, and telecom giants adopted it early and built programs around it to reduce churn and increase customer lifetime value.
Healthcare came later to the game. But rising consumer expectations, tighter margins, and value-based reimbursement models have made NPS a strategic imperative for hospitals and health systems.
And while patient satisfaction metrics abound, NPS does something unique: it focuses on one key behavior—whether patients would recommend your organization to someone else. That recommendation is the heartbeat of reputation, loyalty, and ultimately, growth.
Why NPS Matters in Healthcare
When a patient gives your hospital a 6 out of 10, what are they really saying? Maybe the doctor was kind, but the front desk was cold. Maybe the care was fine, but the experience lacked trust.
That’s why the Net Promoter Score works. It cuts through the noise to one essential question: Would you recommend us?
According to a 2023 study by NRC Health, 60% of healthcare consumers say personal recommendations are a top factor in selecting a provider. And while patient experience (PX) scores may be abstract to some, NPS translates directly to word-of-mouth.
It also has a financial impact. PX scores factor into CMS’s Hospital Value-Based Purchasing program, affecting up to 2% of Medicare reimbursement. Those same PX scores influence Hospital Star Ratings—and each additional star can boost volume by 5–10%.
Hospitals with high NPS scores are not just delivering a better experience. They’re positioning themselves for financial growth, reputation gains, and long-term consumer loyalty.
How NPS Works
NPS is calculated by asking patients one core question:
“On a scale from 0 to 10, how likely are you to recommend our hospital to a friend or family member?”
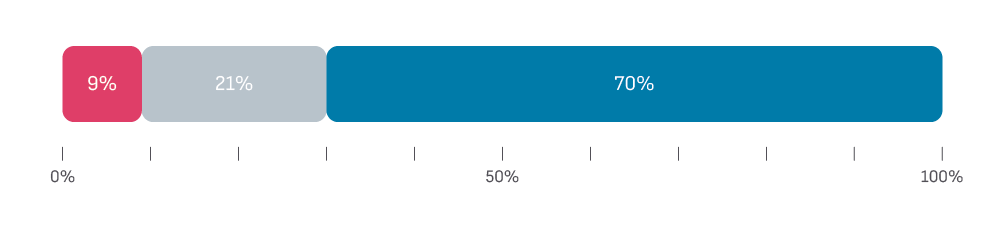
Based on their responses, patients fall into three categories:
Promoters (9–10): Loyal, enthusiastic, likely to recommend.
Passives (7–8): Satisfied, but indifferent—easily wooed by competitors.
Detractors (0–6): Dissatisfied and at risk of spreading negative sentiment.
To calculate your score: subtract the percentage of Detractors from the percentage of Promoters. If 70% are Promoters and 9% are Detractors, your NPS is 61, which is depicted in the graph below.
In healthcare, the average NPS hovers between 30 and 40. Scores over 70 are exceptional—often placing an organization in the top decile for patient experience.
Strategic Uses of NPS in Healthcare
NPS becomes even more powerful when it’s used across departments. When marketing teams collaborate with operations, strategy, and quality teams to interpret and act on NPS data, the results go far beyond branding.
Here’s how NPS can support key strategic priorities:
1. Loyalty & Retention
NPS gives a clear, digestible snapshot of patient loyalty. High scores indicate a strong connection to your brand—fueling retention, referrals, and a stronger reputation.
2. Service Line Growth
Promoters are more likely to return—and more likely to recommend. For marketers, this is where NPS goes from data to action. When you see promoters concentrated in a service line, partner with those clinical leaders. Use that insight to build campaigns around advocacy, loyalty, and brand trust. For services you’re trying to grow, NPS can serve as an early indicator of whether the experience is supporting your growth goals.
3. Experience & Facility Improvements
Supplement the core NPS question with targeted experience feedback—on wait times, communication, facility cleanliness, and scheduling. These insights can guide improvements and help measure their impact over time.
4. Quality & Safety
Detractors often point to breakdowns in care transitions or discharge planning. These insights can guide quality improvement efforts that reduce readmissions, improve HCAHPS scores, and mitigate financial penalties.
5. Competitive Intelligence
Benchmark your NPS against similar organizations. A strong score can validate your positioning in a competitive market. A weak one can help sharpen your marketing message—or highlight internal issues that need attention.
6. Brand & Reputation
What your patients say about you is your brand. NPS offers a feedback loop that’s real-time and actionable, providing both a pulse on reputation and fuel for storytelling. If you’re leading a brand refresh, or targeting growth in a specific region, or after a merger or acquisition, you might be missing the story you need to power your marketing strategy.
7. Alignment with Value-Based Care
Patient experience isn’t just a marketing metric—it’s a measure of value. NPS supports the requirements of value-based care models by tying experience directly to loyalty, which supports quality, cost, and outcomes.
So—Is NPS Really the One Number You Need?
Reichheld claimed that NPS was the one number you needed to grow. Is that still true?
With so many metrics flying around—HCAHPS, CG-CAHPS, CMS star ratings—you might ask, “Do we really need one more number?”
But here’s the truth:
NPS doesn’t just measure satisfaction. It predicts growth.
It tells you whether people will choose you again, and whether they’ll tell others to do the same. In a world where 60% of healthcare decisions are influenced by personal recommendations, that’s not fluff. That’s strategy.
So don’t just collect the score. Use it. Break it down by service line. Track it over time. Build campaigns around your promoters—and fix what turns people into detractors.

Alex Sydnor, FACHE
VP of Marketing and Comm.
As a senior executive, Alex has led healthcare strategy, marketing, patient experience, and population health programs for 17 years. A Fellow of ACHE, he has a Master’s in Hospital Administration and is a trained facilitator. He enjoys hiking & making maple syrup and cider from his home in Maine.